Type of therapies:
Currently several different methods of therapy are used with different functions:
Cervical VNS:
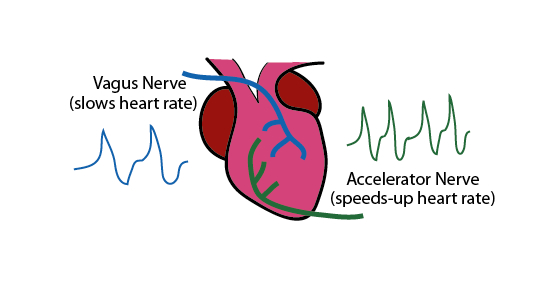
The vagus nerve fibers going down through both sides of the neck. The fibers that go down on the right side innervate the heart and hence this side is used in case of heart failure, but for any other medical conditions the left side is preferred.
Transcutaneous VNS:
A less invasive method is to use that sensation pathway of the ear in order to stimulate the vagus nerve. It usually looks like an earclip attached to the tragus of the ear (left side again, in order to avoid any cardiac involvement) and a mild electric current is sent. The idea behind is that electric current will convey signal from the cutaneous nerve receptors to the brain through the vagus nerve. Another way is done by using a transcutaneous stimulation at the neck area, where the vagus nerve is relatively close to the surface of the skin. A company developed a device called Gammacore, which is now FDA approved to treat migraines using this method.
Other ways:
Enlighten by the anatomical pathways that send signal trough the vagus nerve,other therapies,low tech but efficient can be used as well. Using pahryngeal and learyngeal branches that are responsible for phonation and swallowing, exercises such as humming, gargling, or even gaging (by lighly stroking the epiglottis with a toothbrush for instance) will stimulate the vagus nerve and the nucleus ambiguus. To stimulate the NTS, deep breathing and massage of the abdominal viscera and the carotid body can be helpful.
Vagus Nerve for TBI
In order to understand why vagus nerve stimulation is useful for concussions, let’s have a deeper look into anatomy of the brain and the neuroimmune-endocrine axis. The secret lies into a specific neurotransmitter named acetylcholine. It is the main neurotransmitter involved in the parasympathetic fibers. An interesting property of acetylcholine is that it lowers inflammatory cytokines such as TNF, which is involved in traumatic brain injuries. But acetylcholine is not the only neurotransmitter involved with the vagus nerve. Another neurotransmitter that is enhanced by VNS is norepinephrine, through stimulation of the locus coeruleus (Smith et al.) which is directly correlated with improvement outcome in TBI.
VNS has also shown to enhance GABA production, which is the main inhibitory neurotransmitter of the central nervous system, and to lower GABA’s antagonist, glutamate. This last findings may the the direct reason why TNS attenuates seizures. Another study (George et al 2000) showed that one of the nucleus of the vagus nerve, the nucleus tractus solitarius has a direct connection to other regions of the brain including the insula, the orbitofrontal and prefrontal corices and amygdala. The common point of all those parts of the brain mentioned earlier: they are all very GABA dependant and involved in mood regulation. This explain why vagus nerve stimulation is effective in neuropsychiatric disorders.
A PET scan study (Shi et al. 2015) showed to VNS also increased blood flow in the thalamus, hypothalamus, insular cortex and reticular formation thanks to norepinephrine again. This last area is responsible for arousal and consciousness, which explains why people feel more awake after VNS. Other benefits of norepinephrine include increased cerebral perfusion and hence better oxygenation of the tissues, increased cognitive function, especially in addition with motor training, which seems to enhance neuroplasticity and speed up motor and cognitive rehabilitation process(Pruitt et al 2016). Another part of the brain affected by VNS is the dorsolateral prefrontal cortex, highly involved in working memory and cognitive tasks, and very vulnerable to head injuries (hence those symptoms often show up after a concussion).
Other benefits from VNS are decreased brain edema and tissue damage(Clough et al.), as well as reduction in permeability of the blood brain barrier (often affected after a TBI), probably through anti-inflammatory process as well.
In conclusion, vagus nerve stimulation is improving TBI outcome with the following:
– Decreased inflammation, mainly through cholinergic anti-inflammatory pathway
– Enhanced arousal, level of concsciousness, motor and cognitive function through neuroplasticity
– Decreased in brain edema, tissue damage, blood brain barrier permeability and improvement in cerebral perfusion
– Increased GABA production, and attenuation of glutamate-mediated excitotoxicity.
References
Howland RH. Vagus Nerve Stimulation. Curr Behav Neurosci Rep. 2014;1(2):64-73.
Lopez NE, Krzyzaniak MJ, Costantini TW, Putnam J, Hageny AM, Eliceiri B, Coimbra R, Bansal V. Vagal nerve stimulation decreases blood-brain barrier disruption after traumatic brain injury. J Trauma Acute Care Surg. 2012;72(6):1562–6.
Smith DC, Tan AA, Duke A, Neese SL, Clough RW, Browning RA, Jensen RA. Recovery of function after vagus nerve stimulation initiated 24 hours after fluid percussion brain injury. J Neurotrauma. 2006;23(10):1549–60.
Zhou L, Lin J, Kui G, Zhang J, Yu Y. Neuroprotective effects of vagus nerve stimulation on traumatic brain injury. Neural Regen Res. 2014;9(17):1585–91.
Smith DC, Modglin AA, Roosevelt RW, Neese SL, Jensen RA, Browning RA, Clough RW. Electrical stimulation of the vagus nerve enhances cognitive and motor recovery following moderate fluid percussion injury in the rat. J Neurotrauma. 2005;22(12):1485–502.
Clough RW, Neese SL, Sherill LK, Tan AA, Duke A, Roosevelt RW, Browning RA, Smith DC. Cortical edema in moderate fluid percussion brain injury is attenuated by vagus nerve stimulation. Neuroscience. 2007;147(2):286–93.
Neese SL, Sherill LK, Tan AA, Roosevelt RW, Browning RA, Smith DC, Duke A, Clough RW. Vagus nerve stimulation may protect GABAergic neurons following traumatic brain injury in rats: an immunocytochemical study. Brain Res. 2007;1128(1):157–63.
Neren, D., Johnson, M. D., Legon, W., Bachour, S. P., Ling, G., & Divani, A. A. (2015). Vagus Nerve Stimulation and Other Neuromodulation Methods for Treatment of Traumatic Brain Injury. Neurocritical Care, 24(2), 308–319.
Pruitt DT, Schmid AN, Kim LJ, et al. Vagus Nerve Stimulation Delivered with Motor Training Enhances Recovery of Function after Traumatic Brain Injury. J Neurotrauma.2016;33(9):871-9.
Chen Shi, Steven R. Flanagan, Uzma SamadaniVagus Nerve Stimulation to Augment Recovery from Severe Traumatic Brain Injury Impeding Consciousness: A Prospective Pilot Clinical Trial
Neurol Res. Author manuscript; available in PMC 2015 Sep 14.
Published in final edited form as: Neurol Res. 2013 Apr; 35(3): 263–276.
Martelli D1, McKinley MJ2, McAllen RM3.The cholinergic anti-inflammatory pathway: a critical review. Auton Neurosci. 2014 May;182:65-9.
George, M. S., Sackeim, H. A., Rush, A. J., Marangell, L. B., Nahas, Z., Husain, M. M., … Ballenger, J. C. (2000). Vagus nerve stimulation: a new tool for brain research and therapy∗. Biological Psychiatry, 47(4), 287–295.
Hosoi, T., Okuma, Y., & Nomura, Y. (2000). Electrical stimulation of afferent vagus nerve induces IL-1β expression in the brain and activates HPA axis. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 279(1), R141–R147.
Kelley, K.W., Bluthé, R.-M., Dantzer, R., Zhou, J.-H., Shen, W.-H., Johnson, R.W., 1467 Broussard, S.R., 2003. Cytokine-induced sickness behavior. Brain Behav. Immun. 1468 17 (Suppl. 1), S112–8.)
The Cholinergic Anti-inflammatory Pathway: A Missing Link in Neuroimmunomodulation
Valentin A Pavlov, Hong Wang, Christopher J Czura, Steven G Friedman, Kevin J Tracey
Mol Med. 2003 May-Aug; 9(5-8):125–134
Long Zhou, JinNeuroprotective effects of vagus nerve stimulation on traumatic brain injuryhuang Lin, Junming Lin, Guoju Kui, Jianhua Zhang, Yigang Yu
Neural Regen Res. 2014 Sep 1; 9(17): 1585–1591
